Pivot Office on Cervical Cancer
Second opinion outpatient clinic Please feel free to visit us at our newly opened free consultation outpatient clinic for cervical and vaginal cancer. Services are limited to 30 minutes for patients who bring in documents or test results. We appreciate your understanding.
Cervical cancer
Since H. Zur Hausen identified the human papillomavirus (HPV) as its cause, cervical cancer is the first cancer recognized by the World Health Organization as being 100% caused by HPV infection.
In Japan, 29,136 patients and 6,818 deaths were associated with cervical cancer in 2021. Outside Japan, HPV infection is most common in Africa. It is estimated that 300 million people worldwide are infected with HPV annually. If the current situation continues, it is feared that approximately 44 million people will develop cervical cancer over the next 50 years.
Local therapies such as cryotherapy, electrosurgical loop excision, and laser ablation are considered to be conservative treatments. However, these can cause negative effects, such as bleeding, infection, incomplete and residual resection, uterine stenosis and obstruction, infertility, cervical incompetence, and premature birth, as well as poor sexual quality of life. In addition, in the case of these methods, there have been cases of recurrence due to HPV reinfection even after the primary disease disappeared. In such a case, a total hysterectomy would be the next option, which may lead to a decline in birth rates. This would be a serious problem, not only for obstetrics and gynecology care but also for national policy. In recent trends, cervical cancer starts to increase in women in their 20s and peaks in women in their 30s. In the past, cervical cancer was more common in women in their 40s and older who had married, given birth, and gone through menopause, so treatment at that time would naturally need to change. Cancer is a troublesome disease that affects not only the patient but also those around the patient and deprives a peaceful daily life. For more than 30 years, the author has been researching conservative and sustainable treatments for cervical cancer patients to find treatments adapted to their generation.
Essential points in preventing and treating cervical cancer
Either #1 Elimination of its cause, HPV, or #2 Improvement of abnormal cytology is necessary.
The analysis results for 156 patients were: #1 HPV disappearance rate of 84.6% and #2 98.7% improvement in cytodiagnosis.
Initially, the treatment design aimed at eliminating HPV, but it turned out to be a nice miscalculation as it unexpectedly and markedly improved abnormalities in cytology.
This treatment method was named the Scrape off & Inflammatory reaction (SIR) method in which cells involved in the inflammatory reaction at the squamocolumnar junction, the center of HPV infection, are scraped off with a soft sponge to treat the disease. Although it involves some pain and bleeding, there were no adverse reactions that exceeded its benefits. It does not require large-scale facilities or high costs and can be used in developing countries.
Vaccines
Both preventive and therapeutic vaccines exist, but the latter has not yet been available for HPV. The former is expected to have a high preventive effect, but it is meaningless for people who are already infected.
Among the approximately 200 types of HPV found, there are 13 internationally recognized high-risk HPV types: HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68. Additionally, there are 7 types of HPV: HPV26, 53, 66, 67, 70, 73, and 82, which are rare but have been found in cancer tissue; in total, 20 types are known. The latest 9-valent vaccines, HPV6 and 11, do not cause cancer but are intended to prevent genital warts. Therefore, the 9-valent vaccine’s cancer prevention is effective only against 20 − 7 = 13 types of HPV. We recommend that you understand this point before getting vaccinated. It is because there is a risk that the vaccination may cause people to let their guard down and engage in unintentional sexual intercourse, or they may mistakenly believe that they do not need to undergo cervical cancer screening.
In summary, all women, including men, should be vaccinated at an early age and undergo regular cervical cancer screening after the age of 20. If the vaccine does not prevent infection, or if an infection is confirmed without vaccination, the patient should undergo SIR method treatment if she wishes to conceive or avoid surgery. Alternatively, if she does not want to undergo surgery, she should undergo conventional local therapy.
Case 1: Ms. M.S., 31 years old
Feb. 7, 2019 A clinic in Tokyo
Cytology: LSIL
Mar. 9 First visit to our clinic
HPV(+) index 1)1269.57 Cervix
Aug. 27 HPV(+) index 2569.81 Cervix
Sep. 17 District (ku) screening ASC-US
Sep. 28, 2020 HPV(+) index 1256.28 Cervix
Dec. 9 HPV(+) index 173.54 Vaginal wall
HPV Type 16 Cervix
Types 6, 16 Vaginal wall
HLA2) DRB13) gene Allele14) 040501
Allele2 145401
HLA DQB1 gene Allele1 040101
Allele2 050201
Dec. 16 Start of the Cervical Cancer Control Project treatment
Dec. 28 HPV(−) index 0.25 Cervix
(−) index 0.24 Vaginal wall
Jan. 22, 2021 HPV(−) index 0.20 Cervix
(−) index 0.17 Vaginal wall
Feb. 3 HPV(−) index 0.20 Cervix
(−) index 0.33 Vaginal wall
HPV Type (−)
Cured by treatment of 39 days
Case 2: Ms. K.K., 29 years old
Sep. 13, 2019 A clinic in the UK
HPV Types 16, 51, 52, 56
Jan. 15, 2020 Clinic in Tokyo
Cytology: class Ⅲa/LSIL
Jul. 18 Cytology: class Ⅲa/LSIL
HPV(+)
Nov. 21 Cytology: class Ⅲa/LSIL
Feb. 6, 2021 Cytology: class Ⅲa/ASC-US
Mar. 29 First visit to our clinic
Sep. 14 Clinic in Tokyo Cytology: class Ⅲa/LSIL
Oct. 1 HPV Type (+) 16
Nov. 2 At our clinic
HPV (+) index 80.68 Cervix
(+) index 867.36 Vaginal wall
Type (+)16 Cervix
(+) Types 6, 16 Vaginal wall
HLA A Locus gene Allele1 240201
Allele2 310102
HLA B Locus gene Allele1 390103
Allele2 520101
HLA DRB1 gene Allele1 150101
Allele2 150201
HLA DQB1 gene Allele1 060101
Allele2 060201
Nov. 6 Start of the Cervical Cancer Control Project treatment
Jun. 20, 2022 Cytology: class Ⅱ/ NILM
HPV(−) index 0.24 Cervix
Jul. 5 HPV(−) index 0.26 Cervix
Jul. 26 HPV(−) index 0.24 Cervix
Sep. 27 HPV(−) index 0.29 Vaginal wall
Oct. 14 HPV(−) index 0.45 Vaginal wall
Nov. 5 HPV(−) index 0.34 Vaginal wall
Cured by treatment of 187 days
Comments for Cases 1 and 2
HPV type 6 does not cause cervical cancer but causes warts called anogenital warts, which do not become cancerous but are considered precancerous and should be treated with caution. Juvenile-onset recurrent respiratory papillomatosis, which occurs in children born to infected pregnant women, is difficult to cure and often recurs repeatedly. The effects on the child include speech disturbances and airway narrowing due to the tumor itself, which are similar to post-operative scarring. Some measures must be taken to address the potential damage to both mother and child.
The SIR method allows for avoiding the above risks by eliminating HPV type 6, a cause of the disease.
Case 3: Ms. O.N., 33 years old
Jan. 19, 2019 Pregnant 13 week 4 days
Cytology: class Ⅱ/NILM
HPV(+) index 2716.66 Cervix
July, 2021 Delivery
Mar. 28, 2022 District (ku) screening at our clinic class Ⅱ/NILM
HPV(+) index 18.71 Cervix
Apr. 18 HPV(+) index 32.56 Vaginal wall
HPV Type 58 Cervix
HLA5) A Locus gene Allele1 020701
Allele2 240201
HLA B Locus gene Allele1 152701
Allele2 460101
HLA DRB1 gene Allele1 080302
Allele2 090102
HLA DQB1 gene Allele1 060101
Allele2 030302
Apr. 25 Start of the Cervical Cancer Control Project treatment
Apr. 28 HPV Type 58 Vaginal wall
May. 12 HPV(−) index 0.18 Cervix
HPV(−) index 0.19 Vaginal wall
May. 26 HPV(−) index 0.19 Cervix
HPV(−) index 0.20 Vaginal wall
Jun. 15 HPV(−) index 0.22 Cervix
HPV(−) index 0.20 Vaginal wall
Cured by treatment of 37 days
Case 4: Ms. H.S., 50 years old
Aug. 26, 2021 Clinic in Tokyo
Cytology class Ⅲb/HSIL
Oct. 26 Cytology class Ⅲb/HSIL/CIN2
Nov. 16 HPV Other than Types16, 18
Mar. 24, 2022 Cytology class Ⅲ/ASC-H
Jun. 24 class Ⅲa/ASC-US
Nov. 1 class Ⅲ/ASC-H
Apr. 11, 2023 class Ⅲ/ASC-H
Jun. 21 First visit to our clinic
Jun. 23 Start of the Cervical Cancer Control Project treatment
HPV(−) index 0.23 Cervix
(+) index 1.39 Vaginal wall
HPV Type Unknown if cervix or vaginal wall
HLA A Locus gene Allele1 240201
HLA B Locus gene Allele1 070201
Allele2 460101
HLA DRB1 gene Allele1 040301
Allele2 080302
HLA DQB1 gene Allele1 060101
Allele2 030201
Jul. 1 HPV(−) index 0.18 Cervix
Jul. 26 HPV(−) index 0.63 Cervix
HPV(−) index 0.32 Vaginal wall
Cytology class Ⅱ/NILM
Aug.12 HPV(−) index 0.43 Vaginal wall
Sep. 1 HPV(−) index 0.45 Vaginal wall
Cured by treatment of 44 days
Case 5: Ms. N.N., 52 years old
Nov. 18, 2015 A clinic in Fukuoka/Cytology Moderate dysplasia
Mar. 16, 2017 Cytology Moderate dysplasia
Apr. 25 Cryosurgery
Aug. 22 Cytology Mild dysplasia
Oct. 25 A cancer center/Cytology LSIL Mild dysplasia/HPV Types 16, 33, 56, 58
Dec. 8, 2021 Cytology HSIL Moderate dysplasia
Jun. 30, 2023 First visit to our clinic
Jul. 3 HPV(+) index 31.27 Cervix/(−) index 0.36 Vaginal wall
HLA A Locus gene Allele1 020101
Allele2 240201
HLA B Locus gene Allele1 3904
Allele2 590101
HLA DRB1 gene Allele1 040501
Allele2 080302
HLA DQB1 gene Allele1 060101
Allele2 040101
Start of the Cervical Cancer Control Project treatment
Jul. 18 HPV(−) index 0.57 Cervix
Cytology: Class Ⅱ/NILM
Aug. 8 HPV(−) index0.18 Cervix
Sep. 1 HPV(−) index0.48 Cervix
Cured by treatment of 36 days
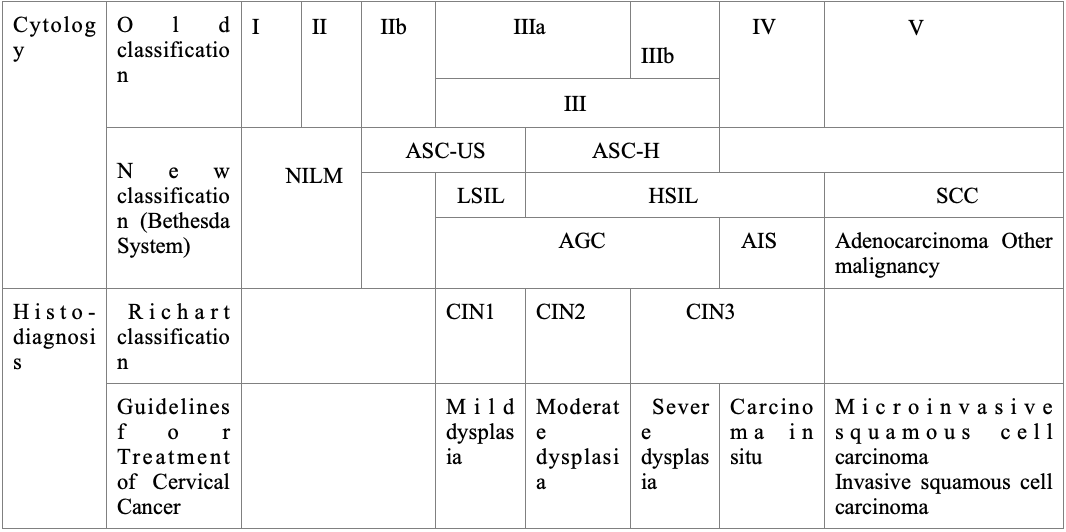
Cytology: Old classification
Class I: Normal
Class II: Suspected benign changes (physiological changes, inflammation, etc.); the possibility of cancer is extremely rare
Class IIb: Suspicion of benign change, but dysplasia (precancerous lesion) cannot be ruled out
Class IIIa/IIIb: Suspicion of dysplasia, slight suspicion of cancer
Class IV: Suspected intraepithelial carcinoma, suspicion of invasive carcinoma
Class V: Cancer (suspected invasive cancer)
Cytology: New classification
Since 2013, the Japanese Association of Obstetricians and Gynecologists and the Ministry of Health, Labor, and Welfare have only been using the Bethesda system.
NILM: Negative for intraepithelial lesion or malignancy
ASC-US: Atypical squamous cells of undetermined significance
ASC-H: Atypical squamous cells, cannot exclude HSIL
LSIL: Low-grade squamous intraepithelial lesion
HSIL: High-grade squamous intraepithelial lesion
SCC: Squamous cell carcinoma
AGC: Atypical glandular cells
AIS: Adenocarcinoma in situ
Histological diagnosis: Richart classification
CIN1: Mild dysplasia
CIN2: Moderate dysplasia
CIN3: Severe dysplasia, intraepithelial carcinoma
As described above, treatment required a mean of 78.9 days.
1) Index (n) represents the degree of infection.
2) HLA (Human leukocyte antigen)
It is used to determine rejection or incompatibility in organ transplantation or blood transfusion.
3) DRB1, DQB1
HLA has classes Ⅰ, Ⅱ, and Ⅲ. Of these, a molecule of class Ⅱ
4) Allele
The designated locus on a pair of opposing chromosomes derived from each parent is called a gene locus (allele). After HPV infection, most of it is naturally excreted. Alleles are tested as to whether cancer development that cannot be excreted is caused by the gene.
5) A, B loci
Molecule belonging to HLA class Ⅰ

